Zoonosis
What is Zoonosis?
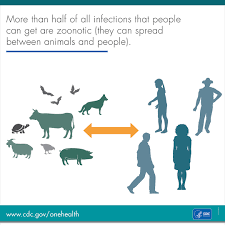
Zoonosis refers to diseases and infections that can be transmitted from animals to humans. These diseases can be caused by a wide range of pathogens, including bacteria, viruses, parasites, and fungi. Zoonotic diseases can be acquired through direct contact with animals, their body fluids, or their waste products, or indirectly through environmental exposures such as contaminated water or food.
Who's at risk for Zoonosis?
Anyone who comes into contact with animals or animal environments is potentially at risk of contracting zoonotic diseases. However, certain groups may be more vulnerable, including:
- People with occupational exposure: Individuals who work closely with animals, such as farmers, veterinarians, animal handlers, or laboratory workers, are at higher risk due to their frequent and close interactions with animals and their biological materials.
- Pet owners: People who have pets, especially those with close contact to animals such as dogs, cats, birds, or reptiles, should be aware of zoonotic risks and take necessary precautions.
- Travelers: People visiting areas with unique animal populations or different zoonotic disease profiles may be at increased risk. Travelers should be informed about potential risks and follow appropriate preventive measures.
- Immunocompromised individuals: Those with weakened immune systems, such as individuals with HIV/AIDS, undergoing chemotherapy, or taking immunosuppressive medications, may be more susceptible to severe or opportunistic zoonotic infections.
What causes Zoonosis?
Zoonotic diseases can be caused by various pathogens that can infect both animals and humans. The sources of zoonotic infections include:
- Bacteria: Examples of zoonotic bacteria include Salmonella, Campylobacter, E. coli, and Leptospira.
- Viruses: Zoonotic viruses include Rabies, Influenza (such as Avian influenza and Swine influenza), and certain types of coronaviruses (e.g., SARS-CoV-2).
- Parasites: Parasitic zoonoses include Toxoplasmosis, Leishmaniasis, Lyme disease (caused by ticks), and Cryptosporidiosis.
- Fungi: Some fungal infections can be zoonotic, such as Histoplasmosis and Ringworm.
The transmission of these pathogens can occur through various routes, including direct contact with infected animals, consumption of contaminated food or water, inhalation of airborne particles, or through vectors like mosquitoes or ticks.
How does Zoonosis start?
Zoonotic diseases typically start when a pathogen is transmitted from an infected animal to a human. This can occur through various means, including:
- Direct contact: Coming into contact with an infected animal's saliva, blood, urine, feces, or other bodily fluids can lead to transmission. This can happen through bites, scratches, handling of animals, or contact with contaminated surfaces.
- Consumption of contaminated food or water: Eating or drinking contaminated animal products, such as undercooked meat, raw eggs, unpasteurized milk, or contaminated water, can result in zoonotic infections.
- Vector-borne transmission: Certain zoonotic diseases are transmitted by vectors such as mosquitoes, ticks, or fleas. The vectors become infected by feeding on infected animals and then transmit the pathogen to humans through subsequent bites.
- Inhalation of airborne particles: Some zoonotic pathogens can be present in the environment, such as in the dust, soil, or feces of infected animals. Inhalation of these particles can lead to respiratory infections.
It's important to note that not all interactions with animals or exposure to zoonotic pathogens will result in infection. The susceptibility to zoonotic diseases depends on various factors, including the specific pathogen, the individual's immune system, and the route and intensity of exposure.
What are the symptoms of Zoonosis?
The symptoms of zoonotic diseases can vary widely depending on the specific pathogen and the individual's immune response. Some common symptoms may include:
- Fever
- Fatigue
- Headache
- Muscle aches
- Gastrointestinal symptoms (nausea, vomiting, diarrhea)
- Respiratory symptoms (cough, shortness of breath)
- Skin rashes or lesions
- Neurological symptoms (seizures, confusion)
The severity of symptoms can range from mild to severe, and some zoonotic infections can lead to life-threatening complications, especially in individuals with weakened immune systems.
How is Zoonosis diagnosed?
The diagnosis of zoonotic diseases requires a thorough medical evaluation by a healthcare professional. The diagnostic process may include:
- Detailed medical history: The healthcare provider will inquire about recent animal exposure, travel history, and specific symptoms.
- Physical examination: A physical examination may help identify any visible signs or symptoms that could be indicative of a zoonotic infection.
- Laboratory tests: Various laboratory tests may be performed, including blood tests, stool or urine analysis, serology (testing for specific antibodies), or molecular tests (such as PCR) to detect the presence of the pathogen.
In some cases, specialized tests or consultation with infectious disease specialists may be necessary for accurate diagnosis.
How can Zoonosis be treated?
The treatment of zoonotic diseases depends on the specific pathogen and the severity of the infection. Treatment options may include:
- Antibiotics: Bacterial zoonotic infections can often be treated with antibiotics, which are prescribed based on the specific bacteria involved and the individual's health status.
- Antiviral medications: Antiviral drugs may be used to treat certain viral zoonotic infections, but their availability and effectiveness can vary depending on the specific virus.
- Antiparasitic medications: Parasitic zoonoses are typically treated with antiparasitic drugs, such as antimalarials or antiparasitic agents, tailored to the specific parasite involved.
- Supportive care: Symptomatic treatment, such as pain relief, hydration, and rest, may be recommended to manage symptoms and support the body's recovery.
It's important to seek medical attention if you suspect a zoonotic infection to receive appropriate treatment and prevent complications.
What complications may occur with Zoonosis?
Complications from zoonotic diseases can vary depending on the specific pathogen involved. Some zoonotic infections can lead to severe illness, organ damage, or long-term health consequences, especially in individuals with weakened immune systems. Examples of potential complications include:
- Pneumonia or respiratory failure
- Meningitis or encephalitis
- Kidney or liver damage
- Cardiac abnormalities
- Chronic or recurring infections
- Development of chronic conditions or autoimmune disorders
Prompt diagnosis, early treatment, and appropriate medical care are essential to minimize the risk of complications.
How can I prevent Zoonosis?
Preventing zoonotic infections involves taking appropriate precautions when interacting with animals and minimizing exposure to potentially contaminated sources. Some preventive measures include:
- Practicing good hygiene: Wash hands thoroughly with soap and water after handling animals, cleaning animal waste, or visiting animal environments. Use hand sanitizers if soap and water are not available.
- Proper food handling: Cook meat thoroughly, avoid cross-contamination of raw and cooked foods, and practice safe food storage and preparation techniques.
- Vaccination: Ensure that pets and livestock receive appropriate vaccinations to prevent certain zoonotic diseases.
- Vector control: Protect yourself from vector-borne zoonotic diseases by using insect repellents, wearing protective clothing, and taking measures to reduce mosquito or tick exposure.
- Safe water and food sources: Drink clean, treated water and consume food from reliable sources to minimize the risk of waterborne or foodborne zoonotic infections.
- Awareness and education: Stay informed about zoonotic diseases prevalent in your area or in regions you plan to visit. Follow public health guidelines and recommendations for disease prevention.
Long-term management of Zoonosis
Long-term management of zoonotic diseases involves ongoing awareness, preventive measures, and regular communication with healthcare professionals. It's important to stay informed about the latest developments and preventive strategies related to zoonoses. Regular veterinary care and preventive measures for pets and livestock are also essential in reducing the risk of zoonotic infections.
What is recent research saying about Zoonosis?
Ongoing research on zoonotic diseases focuses on various aspects, including understanding the transmission dynamics, identifying emerging zoonotic pathogens, developing improved diagnostic methods, and exploring effective prevention and control strategies. In light of recent events, such as the COVID-19 pandemic, there is increased emphasis on zoonotic disease surveillance, early detection, and global collaboration to mitigate the risks of future zoonotic outbreaks.
Where can I go for more information on Zoonosis?
For more information on zoonotic diseases, it is recommended to consult reputable sources such as national and international health organizations, including the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC). These organizations provide comprehensive information, guidelines, and resources related to zoonoses. Additionally, local health departments, veterinarians, and infectious disease specialists can provide specific information and guidance based on your region or circumstances.

