Wilson's Disease
What is Wilson's Disease?
Wilson's disease is a rare genetic disorder characterized by the abnormal accumulation of copper in various organs, especially the liver and brain. It is an autosomal recessive disorder, meaning that individuals inherit the gene mutation from both parents. The excessive copper buildup can cause damage to these organs over time. Wilson's disease is treatable, and with early diagnosis and appropriate management, individuals can live normal lives.
Who's at risk for Wilson's Disease?
Wilson's disease is a hereditary condition, meaning it is passed down through families. It affects both males and females, and the risk is equal among genders. The disorder occurs worldwide, although the prevalence may vary among different populations. Individuals who have a family history of Wilson's disease or who are born to parents with Wilson's disease are at an increased risk of developing the condition.
What causes Wilson's Disease?
Wilson's disease is caused by mutations in the ATP7B gene, which is responsible for producing a protein that transports copper from the liver into bile for elimination. These mutations result in impaired copper transport and lead to the abnormal accumulation of copper in various tissues, particularly the liver and brain. The excess copper buildup can cause liver damage and affect the central nervous system, resulting in a range of symptoms.
How does Wilson's Disease start?
Wilson's disease typically starts during childhood or adolescence, although it can also manifest in adulthood. The accumulation of copper begins early in life but may not cause noticeable symptoms until later stages of the disease. The copper buildup gradually progresses and can result in liver damage, neurological symptoms, or a combination of both.
What are the symptoms of Wilson's Disease?
The symptoms of Wilson's disease can vary widely among individuals and can affect different organs in the body. Common symptoms may include:
- Liver-related symptoms: These may include fatigue, weakness, jaundice (yellowing of the skin and eyes), abdominal pain or swelling, easy bruising or bleeding, and fluid accumulation in the abdomen (ascites) or legs (edema).
- Neurological symptoms: Neurological manifestations can range from mild to severe and may include tremors, difficulty with coordination and balance, slurred speech, muscle stiffness or rigidity, problems with fine motor skills, personality changes, depression, anxiety, or cognitive impairment.
- Eye-related symptoms: Some individuals with Wilson's disease may develop Kayser-Fleischer rings, which are copper deposits that form in the cornea of the eyes. These rings appear as a golden-brownish discoloration around the iris.
- Other symptoms: Additional symptoms may include kidney problems, osteoporosis, anemia, and menstrual irregularities in females.
It's important to note that not all individuals will experience the same symptoms, and the severity can vary.
How is Wilson's Disease diagnosed?
Diagnosing Wilson's disease involves a combination of clinical evaluation, medical history, physical examination, and various diagnostic tests. A healthcare professional, typically a gastroenterologist or hepatologist, may consider the following:
- Medical history and symptoms: The healthcare professional will inquire about symptoms and any family history of Wilson's disease.
- Physical examination: A thorough physical examination may be conducted, including an eye examination to look for the presence of Kayser-Fleischer rings.
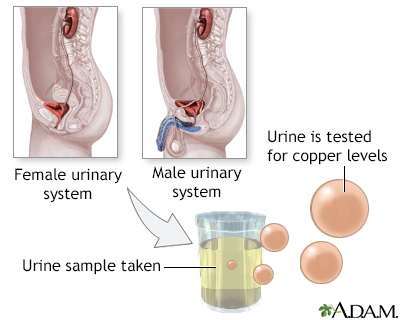
- Blood and urine tests: These tests can measure copper levels, ceruloplasmin (a protein involved in copper transport), and other markers of liver function. Genetic testing may also be performed to identify specific mutations in the ATP7B gene.
- Liver biopsy: In some cases, a small sample of liver tissue may be taken for analysis to assess the copper content and determine the extent of liver damage.
How can Wilson's Disease be treated?
Wilson's disease is a lifelong condition, but with proper treatment, individuals can manage the disease effectively. The primary goal of treatment is to reduce copper buildup and maintain copper levels within a normal range. Treatment options may include:
- Copper chelation therapy: Medications, such as penicillamine, trientine, or zinc acetate, are used to bind excess copper and promote its elimination from the body through urine or stool.
- Zinc supplementation: Zinc blocks the absorption of copper from the digestive tract, reducing the amount of copper absorbed by the body. It is often used as maintenance therapy after initial copper reduction.
- Liver transplantation: In cases of severe liver damage or failure, a liver transplant may be necessary to replace the damaged liver with a healthy one.
Treatment plans are tailored to individual needs, and close monitoring of copper levels and overall health is essential to ensure effective management of the disease.
What complications may occur with Wilson's Disease?
If left untreated, Wilson's disease can lead to various complications, including:
- Liver disease: Chronic copper buildup can result in liver inflammation (hepatitis), fibrosis, cirrhosis, or even liver failure.
- Neurological problems: Untreated Wilson's disease can cause significant neurological damage, leading to movement disorders, cognitive impairment, psychiatric symptoms, and disability.
- Kidney damage: Copper accumulation can affect kidney function and lead to renal problems.
- Bone and joint issues: Osteoporosis, osteoarthritis, and other bone-related complications can occur due to copper-induced changes in bone metabolism.
Early detection and appropriate treatment can help prevent or minimize these complications.
How can I prevent Wilson's Disease?
Wilson's disease is an inherited condition, and there is currently no way to prevent its development. However, genetic counseling and testing may be recommended for individuals with a family history of Wilson's disease or those planning to have children. Genetic counseling can provide information about the risks, inheritance patterns, and reproductive options available.
Long-term management of Wilson's Disease
Long-term management of Wilson's disease involves:
- Regular follow-up visits: Ongoing monitoring by a healthcare professional is crucial to assess liver function, copper levels, and overall health.
- Compliance with treatment: Adhering to prescribed medications and treatment plans is essential to maintain copper balance and prevent disease progression.
- Dietary modifications: A low-copper diet may be recommended, which includes avoiding foods rich in copper, such as liver, shellfish, chocolate, nuts, and mushrooms.
- Genetic counseling: Individuals with Wilson's disease and their families may benefit from genetic counseling to understand the inheritance pattern, genetic testing options, and family planning considerations.
What is recent research saying about Wilson's Disease?
Research on Wilson's disease focuses on various aspects, including improved understanding of the underlying genetic mutations, new treatment approaches, and strategies to enhance diagnosis and disease management. Recent studies have explored the use of new chelating agents, targeted gene therapies, and novel diagnostic techniques to enhance early detection and optimize treatment outcomes.
Where can I go for more information on Wilson's Disease?
For more information on Wilson's disease, you can consult reliable sources such as the Mayo Clinic, the Wilson Disease Association, or other reputable medical websites. Additionally, healthcare professionals specializing in liver diseases and genetic disorders can provide comprehensive information and support specific to your individual circumstances.

