Vitiligo
What is Vitiligo?
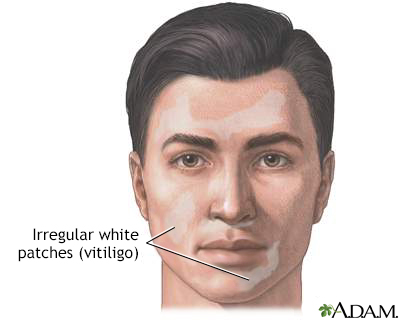
Vitiligo is a chronic skin condition characterized by the loss of skin pigment, resulting in irregular white patches on the skin. It occurs when melanocytes, the cells responsible for producing skin pigment called melanin, are destroyed or unable to function properly. Vitiligo can affect any part of the body, including the skin, hair, and mucous membranes.
Who's at risk for Vitiligo?
Vitiligo can affect individuals of all ages, races, and genders. However, certain factors may increase the risk of developing vitiligo, including:
- Family history: Having a family history of vitiligo or other autoimmune diseases, such as thyroid disease or type 1 diabetes, increases the risk.
- Autoimmune conditions: Individuals with other autoimmune conditions are more likely to develop vitiligo.
- Skin type: People with darker skin types are at a higher risk of developing vitiligo, as the contrast between the depigmented patches and the surrounding skin is more noticeable.
- Certain factors: Certain triggers, such as physical or emotional stress, sunburn, exposure to certain chemicals, or trauma to the skin, may increase the risk or trigger the onset of vitiligo.
What causes Vitiligo?
The exact cause of vitiligo is still unknown. However, it is believed to be an autoimmune condition, in which the immune system mistakenly attacks and destroys the melanocytes in the skin. Several theories suggest possible causes, including genetic factors, an imbalance in the immune system, oxidative stress, or a combination of genetic and environmental factors. However, more research is needed to fully understand the underlying mechanisms.
How does Vitiligo start?
Vitiligo usually begins with the appearance of small, pale or white patches on the skin. These patches often start in areas exposed to the sun, such as the face, hands, arms, feet, and lips. Over time, the patches may enlarge and spread to other areas of the body. The progression of vitiligo can vary from person to person, with some individuals experiencing slow, gradual spreading, while others may have more rapid progression.
What are the symptoms of Vitiligo?
The main symptom of vitiligo is the development of depigmented or white patches on the skin. These patches are more noticeable in individuals with darker skin. The patches may be small and scattered initially but can enlarge and merge over time, resulting in larger areas of depigmentation. Vitiligo can also affect the hair, causing premature graying or loss of color in the affected areas. In some cases, vitiligo may also involve the mucous membranes, such as the inside of the mouth or the genital area.
How is Vitiligo diagnosed?
A dermatologist or healthcare professional can diagnose vitiligo based on a physical examination of the skin, medical history, and a discussion of symptoms. In some cases, additional tests may be performed to rule out other conditions and confirm the diagnosis. These tests may include:
- Wood's lamp examination: A special lamp that emits ultraviolet (UV) light is used to examine the skin. In vitiligo, the affected areas may appear more pronounced under UV light.
- Skin biopsy: A small sample of skin may be taken for laboratory analysis to confirm the absence of melanocytes and rule out other skin conditions.
- Blood tests: Blood tests may be ordered to evaluate thyroid function, detect autoantibodies, or assess the overall immune system.
How can Vitiligo be treated?
Although there is currently no cure for vitiligo, several treatment options are available to help manage the condition and improve the appearance of the skin. Treatment approaches may include:
- Topical corticosteroids: These medications are applied directly to the affected areas of the skin to help reduce inflammation and repigment the skin.
- Topical calcineurin inhibitors: These medications, such as tacrolimus or pimecrolimus, are applied to the skin and can help suppress the immune response and promote repigmentation.
- Topical calcipotriene: This vitamin D derivative may be used in combination with other treatments to help repigment the skin.
- Topical psoralen plus ultraviolet A (PUVA): This treatment combines the application of a psoralen medication and exposure to UVA light to stimulate repigmentation of the skin.
- Narrowband ultraviolet B (NB-UVB) phototherapy: Exposure to specific wavelengths of UVB light can help stimulate the production of melanocytes and repigment the skin.
- Excimer laser: This targeted laser therapy delivers UVB light to specific areas of the skin to promote repigmentation.
- Depigmentation: In cases where vitiligo affects a large portion of the body, depigmentation may be an option to lighten the remaining skin so that it matches the depigmented areas.
The choice of treatment depends on various factors, including the extent of vitiligo, the location of the depigmented patches, and the individual's preferences and goals. It's important to discuss treatment options with a dermatologist or healthcare professional specializing in vitiligo to determine the most appropriate approach.
What complications may occur with Vitiligo?
Vitiligo itself is not a life-threatening condition and does not pose significant health risks. However, it can have emotional and psychological impacts, especially in individuals with visible depigmented patches. The condition may affect self-esteem, body image, and quality of life. It's important to seek support from healthcare professionals, support groups, or counseling services to address any emotional challenges associated with vitiligo.
How can I manage Vitiligo in the long term?
Managing vitiligo involves a combination of treatment approaches and lifestyle strategies. Some strategies that can help in the long-term management of vitiligo include:
- Sun protection: Protecting the skin from excessive sun exposure is important, as sunburn can worsen depigmented patches and increase the risk of skin damage. Sunscreens with a high sun protection factor (SPF) should be used, and protective clothing or hats should be worn when in the sun.
- Camouflage techniques: Cosmetics or skin dyes can be used to help camouflage depigmented areas and improve the appearance of the skin.
- Emotional support: Seeking emotional support from healthcare professionals, support groups, or counseling services can help individuals cope with the emotional and psychological impacts of vitiligo.
- Self-care and self-acceptance: Practicing self-care, maintaining a positive mindset, and accepting oneself can play a significant role in managing the emotional aspects of living with vitiligo.
Regular follow-up appointments with a dermatologist or healthcare professional specializing in vitiligo are important to monitor the condition, adjust treatment as needed, and address any concerns.
What is recent research saying about Vitiligo?
Ongoing research in vitiligo aims to improve our understanding of the underlying mechanisms, develop new treatment options, and identify potential ways to prevent or halt the progression of the condition. Some areas of research include:
- Immunomodulatory therapies: Investigating new medications that can help modulate the immune response in vitiligo and potentially promote repigmentation.
- Stem cell therapies: Exploring the use of stem cells to repopulate the skin with melanocytes and restore skin pigmentation.
- Genetic studies: Investigating the genetic factors associated with vitiligo to better understand the risk factors and potential targets for treatment.
- Psychological impact: Researching interventions and support systems that can help individuals cope with the psychological impacts of vitiligo and improve quality of life.
Where can I go for more information on Vitiligo?
For more information on vitiligo, reliable sources such as the American Academy of Dermatology (AAD), the Vitiligo Society, the Mayo Clinic, or other reputable dermatology organizations and healthcare institutions can provide valuable information and resources. Consulting with a dermatologist or healthcare professional specializing in vitiligo can also provide personalized information and guidance specific to an individual's situation.

