Trigeminal Neuralgia
What is Trigeminal Neuralgia?
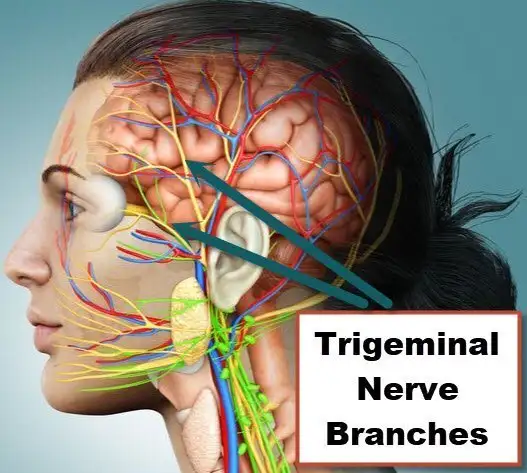
Trigeminal neuralgia, also known as tic douloureux, is a chronic pain disorder that affects the trigeminal nerve, which is responsible for transmitting sensations from the face to the brain. It is characterized by sudden and severe facial pain that can be triggered by even mild stimuli such as touching the face, chewing, speaking, or cold air. The pain is often described as electric shocks or stabbing sensations and typically affects one side of the face. Trigeminal neuralgia can be debilitating and significantly impact a person's quality of life.
Who's at risk for Trigeminal Neuralgia?
Trigeminal neuralgia can affect individuals of any age, but it is more commonly seen in older adults, particularly those over the age of 50. Women are slightly more likely to develop the condition than men. Although the exact cause is unknown, certain factors may increase the risk of trigeminal neuralgia. These include having a family history of the condition, certain medical conditions such as multiple sclerosis, and previous facial trauma or nerve damage.
What causes Trigeminal Neuralgia?
Trigeminal neuralgia is primarily caused by compression or irritation of the trigeminal nerve. This compression can occur due to various factors, including blood vessels pressing on the nerve, the presence of a tumor or cyst in the vicinity, or structural abnormalities in the skull. In some cases, the cause of trigeminal neuralgia is unknown, and it is classified as idiopathic. The compression or irritation of the nerve leads to abnormal firing of pain signals, resulting in the characteristic facial pain associated with the condition.
How does Trigeminal Neuralgia start?
Trigeminal neuralgia typically starts with sudden, severe, and recurring facial pain episodes. These episodes may last for a few seconds to a couple of minutes and are often triggered by ordinary daily activities that involve contact with the face or mouth, such as eating, talking, or brushing teeth. The pain can be intense and debilitating, causing individuals to avoid activities that may trigger an episode. Trigeminal neuralgia can start gradually and worsen over time, with periods of remission and flare-ups.
What are the symptoms of Trigeminal Neuralgia?
The main symptom of trigeminal neuralgia is severe facial pain. The pain is usually localized to one side of the face and can affect different areas supplied by the trigeminal nerve, including the cheek, jaw, teeth, gums, or eye area. The pain is typically described as sudden, sharp, and electric shock-like. It may be triggered by even mild stimuli such as touching the face, talking, or eating. Between episodes, individuals may be pain-free, but the fear of triggering an episode can cause anxiety and impact daily activities.
How is Trigeminal Neuralgia diagnosed?
Diagnosing trigeminal neuralgia involves a thorough evaluation of symptoms, medical history, and a neurological examination by a healthcare professional. The healthcare provider will inquire about the characteristics of the pain, triggers, and associated symptoms. A physical examination will be conducted to assess facial sensation, reflexes, and muscle strength. Imaging tests, such as magnetic resonance imaging (MRI), may be ordered to rule out underlying structural causes or to identify potential compression of the trigeminal nerve.
How can Trigeminal Neuralgia be treated?
The treatment of trigeminal neuralgia aims to relieve pain and improve quality of life. Treatment options may include:
- Medications: Anticonvulsant medications, such as carbamazepine or gabapentin, are often prescribed to control pain and reduce the frequency of episodes. Other medications, such as muscle relaxants or tricyclic antidepressants, may also be used to help manage pain.
- Nerve blocks: Local anesthetic injections or nerve blocks can provide temporary pain relief by numbing the affected area or interrupting the pain signals transmitted by the trigeminal nerve.
- Surgery: In cases where medication or other conservative measures fail to provide adequate relief, surgical interventions may be considered. Procedures such as microvascular decompression, radiofrequency ablation, or gamma knife radiosurgery aim to alleviate nerve compression and reduce pain.
- Complementary therapies: Some individuals find relief from complementary therapies such as acupuncture, biofeedback, or relaxation techniques. These approaches may help manage pain and improve overall well-being. It is essential to consult with a healthcare professional before pursuing complementary therapies.
What complications may occur with Trigeminal Neuralgia?
Trigeminal neuralgia can have significant impacts on an individual's quality of life and daily functioning. The pain can be severe and disabling, leading to difficulty in performing routine activities such as eating, speaking, or personal hygiene. The fear of triggering an episode of pain can cause anxiety and social isolation. The use of pain medications may have side effects, and long-term reliance on medication may pose challenges. Prompt diagnosis and appropriate management can help minimize complications and improve overall well-being.
How can I prevent Trigeminal Neuralgia?
Since the exact cause of trigeminal neuralgia is often unknown, there are no specific preventive measures to avoid its development. However, maintaining overall good health and minimizing factors that can contribute to nerve irritation or compression may be helpful. This includes managing underlying medical conditions, avoiding facial trauma, and practicing stress reduction techniques. Regular check-ups with a healthcare professional can help monitor any potential changes or symptoms that may indicate trigeminal neuralgia.
Long-term management of Trigeminal Neuralgia
Long-term management of trigeminal neuralgia involves working closely with healthcare professionals to find the most effective treatment approach for pain control and symptom management. This may include medication adjustments, regular follow-up appointments, and monitoring of symptoms. Developing strategies to manage pain triggers and practicing stress reduction techniques can also be beneficial. Support from healthcare providers, pain management specialists, and support groups can provide valuable resources and guidance for individuals living with trigeminal neuralgia.
What is recent research saying about Trigeminal Neuralgia?
Recent research on trigeminal neuralgia has focused on improving the understanding of its underlying causes and identifying more effective treatment options. Advances in imaging technology have provided insights into the structural abnormalities associated with the condition, helping to guide treatment decisions. Researchers are exploring new medications and drug delivery methods to target the underlying mechanisms of trigeminal neuralgia and provide more targeted pain relief. Additionally, studies are investigating the role of non-invasive brain stimulation techniques, such as transcranial magnetic stimulation (TMS), as potential treatment options for trigeminal neuralgia.
Where can I go for more information on Trigeminal Neuralgia?
For more information on trigeminal neuralgia, reliable sources such as the Facial Pain Association (formerly the Trigeminal Neuralgia Association), the American Academy of Neurology, or reputable neurology and pain management organizations can provide valuable information and resources. These organizations offer comprehensive information on trigeminal neuralgia, including educational materials, support networks, and ongoing research updates. Consulting with a healthcare professional, such as a neurologist or pain specialist, can also provide personalized information and guidance specific to an individual's situation.

