Thalassemia
What is Thalassemia?
Thalassemia is a group of inherited blood disorders that affect the production of hemoglobin, a protein responsible for carrying oxygen throughout the body. People with thalassemia have an abnormality in the genes that control the production of hemoglobin, leading to reduced production or abnormal structure of the protein. Thalassemia can range from mild to severe and can cause anemia, fatigue, and other complications depending on the type and severity of the condition.
Who's at risk for Thalassemia?
Thalassemia is most commonly found in people of Mediterranean, Middle Eastern, Southeast Asian, and African descent. Individuals with a family history of thalassemia are at a higher risk of inheriting the disorder. Thalassemia is an autosomal recessive condition, meaning both parents must carry the abnormal genes for a child to develop thalassemia. However, individuals from any ethnic background can be carriers of thalassemia genes.
What causes Thalassemia?
Thalassemia is caused by mutations in the genes that control the production of hemoglobin. These mutations affect the synthesis of either the alpha or beta chains of hemoglobin, resulting in reduced production or abnormal structure of the protein. The severity of thalassemia depends on the specific gene mutations involved. In alpha thalassemia, multiple gene mutations are responsible, while in beta thalassemia, mutations occur in a single gene.
How does Thalassemia start?
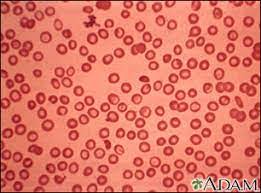
Thalassemia starts when an individual inherits abnormal genes from both parents. The specific gene mutations interfere with the normal production of hemoglobin, resulting in decreased or abnormal hemoglobin in the red blood cells. This leads to a disruption in the structure and function of the red blood cells, causing anemia and related symptoms.
What are the symptoms of Thalassemia?
The symptoms of thalassemia can vary depending on the type and severity of the condition. Individuals with thalassemia may experience fatigue, weakness, pale or yellowish skin, shortness of breath, dizziness, delayed growth and development in children, and an enlarged spleen. Severe forms of thalassemia, such as beta thalassemia major or Cooley's anemia, can lead to life-threatening complications, including severe anemia, bone deformities, and organ damage.
How is Thalassemia diagnosed?
Thalassemia is diagnosed through a combination of physical examination, medical history review, and laboratory tests. Blood tests are used to measure the levels of hemoglobin and red blood cells, as well as to identify specific hemoglobin variants. Additional tests, such as genetic testing or DNA analysis, may be conducted to confirm the presence of specific gene mutations associated with thalassemia.
How can Thalassemia be treated?
The treatment of thalassemia depends on the type and severity of the condition. In milder forms, regular monitoring of the condition may be sufficient, with occasional blood transfusions to manage anemia when necessary. Individuals with more severe forms of thalassemia may require regular blood transfusions to maintain adequate hemoglobin levels. Iron chelation therapy may be necessary to remove excess iron from the body due to repeated transfusions. In some cases, stem cell transplantation or gene therapy may be considered as potential curative treatments.
What complications may occur with Thalassemia?
Thalassemia can lead to various complications, particularly in individuals with more severe forms of the condition. These complications may include iron overload due to repeated blood transfusions, which can affect the heart, liver, and other organs. Enlargement of the spleen (splenomegaly) can occur, leading to hypersplenism and increased susceptibility to infections. Severe anemia can result in delayed growth and development in children and may require regular transfusions for survival.
How can I prevent Thalassemia?
Thalassemia is primarily a genetic condition, and it cannot be entirely prevented. However, genetic counseling and prenatal testing can help identify individuals who carry thalassemia genes, allowing for informed family planning decisions. In areas where thalassemia is more prevalent, such as certain ethnic communities, premarital screening programs and education about carrier status can help reduce the incidence of thalassemia by promoting informed choices and genetic counseling.
Long-term management of Thalassemia
Long-term management of thalassemia involves regular monitoring, appropriate treatment, and support for individuals and families affected by the condition. This includes regular check-ups to monitor hemoglobin levels, organ function, and any potential complications. Adherence to treatment plans, such as blood transfusions or chelation therapy, is essential to manage symptoms and prevent complications. Ongoing support from healthcare providers, including specialists in hematology and genetic counseling, can assist in addressing physical, emotional, and social aspects of living with thalassemia.
What is recent research saying about Thalassemia?
Recent research on thalassemia has focused on developing innovative treatments such as gene therapy and gene editing techniques to correct the genetic mutations responsible for the condition. Advancements in stem cell transplantation and hematopoietic cell gene therapy offer potential curative approaches for individuals with severe thalassemia. Additionally, studies continue to investigate new iron chelation therapies, improved monitoring techniques, and strategies to optimize the quality of life for individuals living with thalassemia.
Where can I go for more information on Thalassemia?
For more information on thalassemia, reliable sources such as the Thalassemia International Federation (TIF), Centers for Disease Control and Prevention (CDC), or reputable medical centers specializing in thalassemia care can provide valuable information and resources. These organizations offer comprehensive information on thalassemia, including support networks, treatment guidelines, ongoing research, and opportunities for patient advocacy. Local healthcare providers, hematologists, and genetic counselors can also serve as important sources of information and support for individuals seeking specific guidance and management strategies for thalassemia.

