Glomerulonephritis
Glomerulonephritis is a kidney disease that affects many people worldwide.
What is glomerulonephritis?
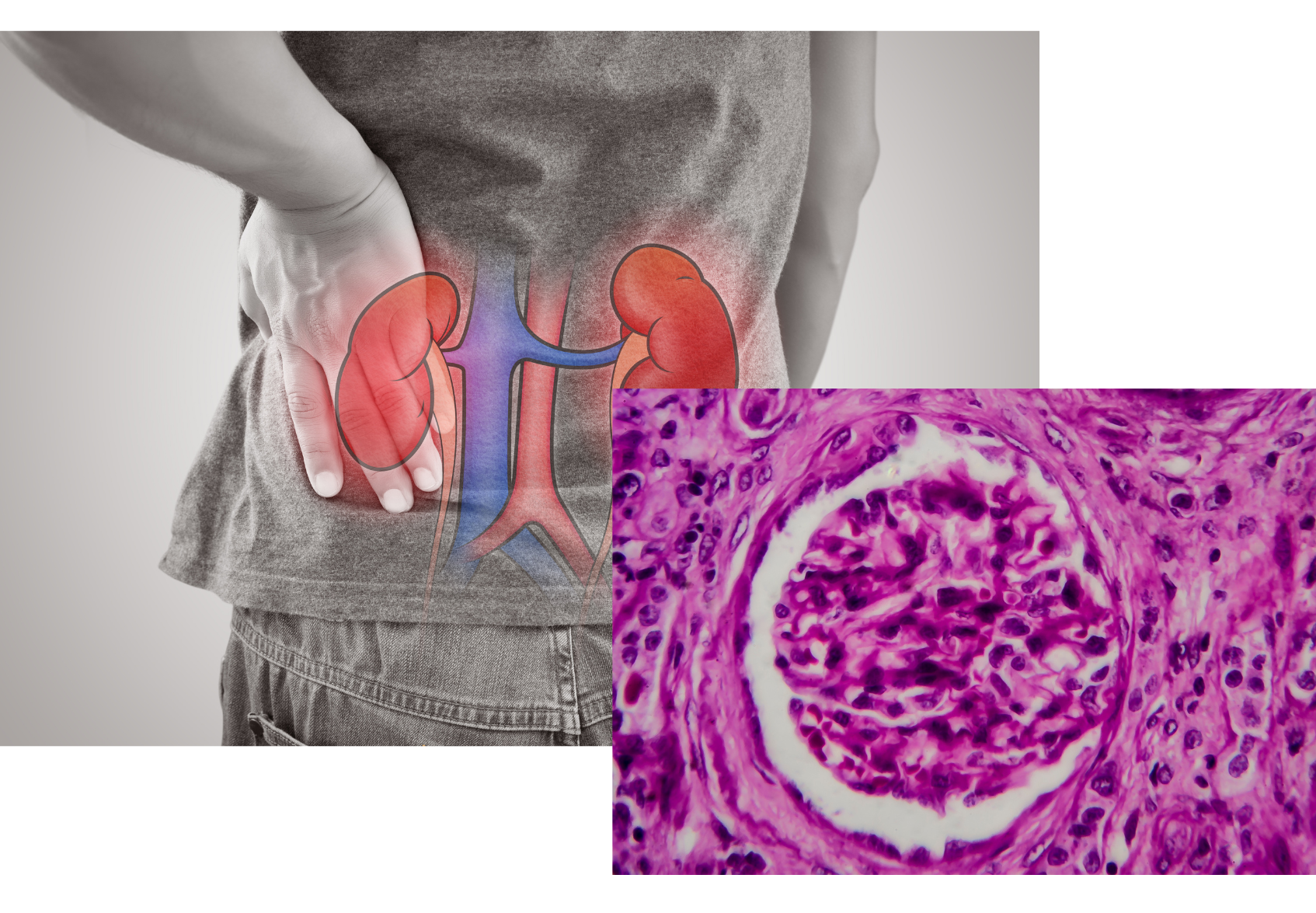
Glomerulonephritis is a group of kidney disorders characterized by inflammation of the glomeruli, the tiny blood vessels in the kidneys responsible for filtering waste and excess fluids from the blood to form urine. This inflammation can impair kidney function and may ultimately lead to kidney failure if left untreated.
Who’s at risk for glomerulonephritis?
People with a family history of kidney disease, a history of autoimmune disorders, or certain infections are at an increased risk of developing glomerulonephritis. Other risk factors include:
- Age: Glomerulonephritis can affect people of all ages but is more common in children and young adults.
- Ethnicity: Some ethnic groups, such as African Americans and Asians, have a higher risk of certain types of glomerulonephritis.
- Sex: Men are more likely to develop glomerulonephritis than women.
What causes glomerulonephritis?
Glomerulonephritis can be caused by various factors, including:
- Infections, such as strep throat, hepatitis B and C, or HIV
- Autoimmune diseases, like lupus or Goodpasture syndrome
- Vasculitis, an inflammation of blood vessels
- Genetic factors, such as Alport syndrome or IgA nephropathy
- Medications, including certain nonsteroidal anti-inflammatory drugs (NSAIDs) and antibiotics
How does glomerulonephritis start?
Glomerulonephritis typically begins when an infection or an autoimmune response triggers inflammation in the glomeruli. This inflammation can cause the glomeruli to become damaged, leading to impaired kidney function and reduced waste and fluid filtration.
What are the symptoms of glomerulonephritis?
Symptoms of glomerulonephritis can vary and may include:
- Swelling (edema) in the face, hands, feet, or abdomen
- Dark or foamy urine
- Fatigue and weakness
- High blood pressure
- Decreased urine output
- Blood in the urine (hematuria)
- How is glomerulonephritis diagnosed?
Glomerulonephritis is diagnosed through a combination of physical examination, medical history, and laboratory tests, such as:
- Urinalysis to detect blood, protein, and other abnormalities in the urine
- Blood tests to measure kidney function and assess electrolyte levels
- Imaging tests, such as ultrasound or CT scan, to evaluate kidney size and structure
- Kidney biopsy to examine a small tissue sample for signs of inflammation and damage
How can glomerulonephritis be treated?
Treatment for glomerulonephritis depends on the underlying cause and severity of the condition. Some treatment options may include:
- Medications to control high blood pressure and reduce inflammation, such as angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), or corticosteroids
- Immunosuppressive drugs to treat autoimmune-related glomerulonephritis
- Antibiotics for infection-related glomerulonephritis
- Dietary modifications, including reduced salt, protein, and potassium intake
- Dialysis or kidney transplant for severe cases or end-stage kidney disease
- What complications may occur with glomerulonephritis?
If left untreated, glomerulonephritis can lead to various complications, including:
- Chronic kidney disease, which can progress to end-stage kidney failure, requiring dialysis or a kidney transplant
- High blood pressure, which can further damage the kidneys and increase the risk of heart disease and stroke
- Nephrotic syndrome, characterized by high levels of protein in the urine, low levels of protein in the blood, and swelling (edema)
- Acute kidney injury, a sudden loss of kidney function that may be reversible with prompt treatment
How can I prevent glomerulonephritis?
Preventing glomerulonephritis depends on addressing the underlying causes and risk factors. Some general prevention tips include:
- Prompt treatment of infections, such as strep throat or skin infections, to reduce the risk of post-infectious glomerulonephritis
- Managing autoimmune diseases and closely monitoring your condition with your healthcare provider
- Regular check-ups and kidney function tests if you have a family history of kidney disease
- Avoiding or using caution with medications that may cause kidney damage
Long-term management of glomerulonephritis
Long-term management of glomerulonephritis involves ongoing medical care, including regular monitoring of kidney function, blood pressure, and electrolyte levels. Adherence to prescribed medications and lifestyle modifications, such as a healthy diet, exercise, and stress reduction, can help improve kidney function and overall health.
What is recent research saying about glomerulonephritis?
Recent research on glomerulonephritis has focused on understanding the underlying causes, improving diagnostic tools, and developing new treatment options. Studies have explored the genetic and molecular mechanisms involved in glomerulonephritis, as well as the role of the immune system in disease progression. Additionally, new medications and therapies, such as stem cell transplantation and targeted immunotherapies, are being investigated for their potential to treat glomerulonephritis and minimize complications.
Where can I go for more information on glomerulonephritis?
If you are looking for more information on glomerulonephritis or need support, consider reaching out to your healthcare provider or a qualified medical professional. They can provide guidance based on your specific situation and answer any questions you may have. Reputable online resources, such as the National Kidney Foundation, the American Kidney Fund, and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), can also offer valuable information and support for those affected by glomerulonephritis.

