Fetal Distress
Fetal distress is a term that has been widely used to describe a range of complications that may arise during pregnancy, labor, or delivery. In this article, we aim to provide a thorough understanding of fetal distress by addressing a set of common questions related to the condition.
What is fetal distress?
Fetal distress refers to a situation where the fetus is not receiving adequate oxygen during pregnancy, labor, or delivery. It can lead to various complications, including developmental issues, brain damage, or even stillbirth if not promptly addressed. Fetal distress is often indicated by abnormal heart rate patterns or reduced fetal movement, among other factors.
Who’s at risk for fetal distress?
There are several factors that may increase the risk of fetal distress, including:
- Advanced maternal age
- Obesity
- High blood pressure or preeclampsia
- Gestational diabetes
- Multiple pregnancies (twins, triplets, etc.)
- Intrauterine growth restriction (IUGR)
- Pre-existing medical conditions
- Substance abuse (smoking, alcohol, or drug use)
- Prolonged labor
What causes fetal distress?
Fetal distress can be caused by various factors that may compromise the oxygen supply to the fetus, such as:
- Problems with the placenta (e.g., placental abruption or insufficiency)
- Umbilical cord complications (e.g., cord compression, prolapse, or knots)
- Uterine rupture or an overly distended uterus
- Infection
- Maternal medical conditions, such as heart or lung disease
- Certain medications
How does fetal distress start?
Fetal distress can begin at any stage of pregnancy, labor, or delivery. It may result from a combination of factors that affect the fetus's oxygen supply or the mother's ability to deliver oxygen-rich blood to the fetus. Early detection and intervention are crucial in minimizing the risks associated with fetal distress.
What are the symptoms of fetal distress?
Some possible signs of fetal distress include:
- Abnormal fetal heart rate (either too fast or too slow)
- Reduced fetal movement
- Meconium-stained amniotic fluid (greenish or brownish color)
- Maternal bleeding or severe abdominal pain
How is fetal distress diagnosed?
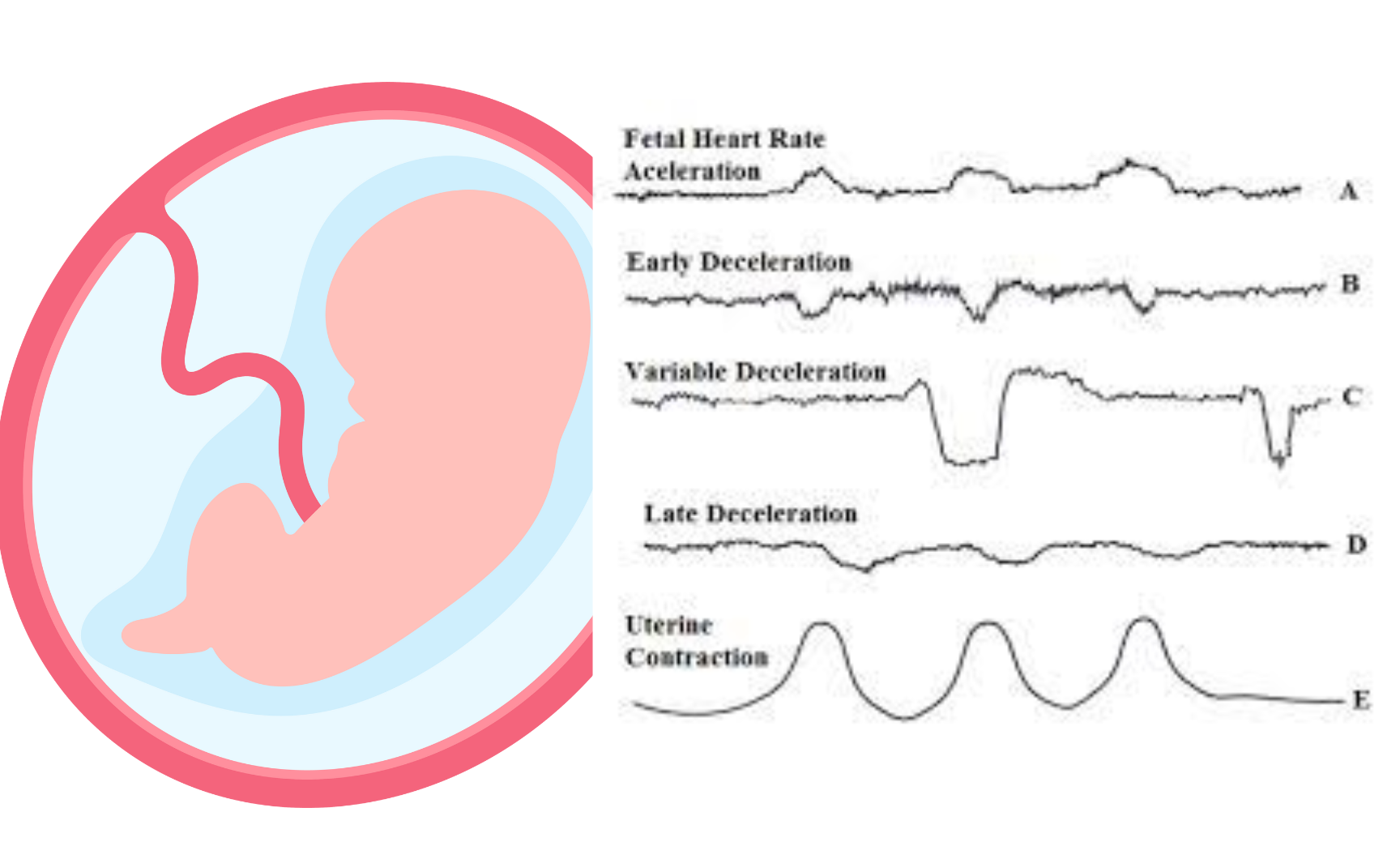
Fetal distress is typically diagnosed through the monitoring of the fetal heart rate, either with a Doppler device or an electronic fetal monitor. If abnormal heart rate patterns are detected, additional tests may be performed, such as a biophysical profile or a fetal scalp pH test to assess the baby's oxygen levels.
How can fetal distress be treated?
The treatment for fetal distress depends on the severity of the condition and the stage of pregnancy or labor. Some possible interventions include:
- Changing the mother's position to improve blood flow to the fetus
- Administering oxygen to the mother
- Hydrating the mother intravenously
- Administering medications to control contractions or blood pressure
- Performing an emergency cesarean section if necessary
- What complications may occur with fetal distress?
If not promptly addressed, fetal distress can lead to severe complications, such as:
- Brain damage due to lack of oxygen
- Developmental delays
- Cerebral palsy
- Hypoxic-ischemic encephalopathy (HIE)
- Stillbirth
How can I prevent fetal distress?
While not all cases of fetal distress can be prevented, taking certain steps may help reduce the risk:
- Regular prenatal care to monitor the health of the fetus and mother
- Maintaining a healthy lifestyle during pregnancy (e.g., balanced diet, exercise, and avoiding smoking, alcohol, and drugs)
- Managing pre-existing medical conditions and closely following your healthcare provider's recommendations
- Reporting any concerns or changes in fetal movement to your healthcare provider immediately
- Learning and practicing relaxation techniques to help cope with stress during pregnancy
Long-term management of fetal distress
The long-term management of fetal distress depends on the severity of the condition and any complications that may have arisen. In cases where a baby has suffered brain damage or developmental delays, ongoing medical care, therapy, and support may be necessary to address the child's needs and improve their quality of life.
What is recent research saying about fetal distress?
Recent research on fetal distress has focused on improving diagnostic tools, refining treatment protocols, and understanding the long-term outcomes for affected infants. Some studies have explored the use of new monitoring technologies to provide more accurate and timely detection of fetal distress. Additionally, research has also investigated the potential benefits of using alternative delivery methods, such as vacuum extraction or forceps, to reduce the risk of complications associated with fetal distress.
Where can I go for more information on fetal distress?
If you are concerned about fetal distress or would like more information, consult your healthcare provider or a qualified medical professional. They can provide guidance based on your specific situation and answer any questions you may have. Additionally, reputable online resources such as the American Pregnancy Association, the March of Dimes, and the Centers for Disease Control and Prevention (CDC) can offer valuable information and support for those affected by fetal distress.

