Urinary Incontinence
What is Urinary Incontinence?
Urinary incontinence refers to the involuntary loss of urine, leading to an inability to control urinary bladder function. It is a common condition that can vary in severity, ranging from occasional leakage to a complete inability to hold urine. Urinary incontinence can significantly impact a person's quality of life, causing embarrassment, social withdrawal, and psychological distress. However, it is important to note that urinary incontinence is not a normal part of aging and can often be treated or managed.
Who's at risk for Urinary Incontinence?
Urinary incontinence can affect individuals of all ages and genders, but certain factors may increase the risk. These include:
- Age: As individuals age, the risk of developing urinary incontinence tends to increase. This can be due to natural changes in the muscles and tissues of the urinary system, as well as age-related medical conditions.
- Gender: Women are more likely to experience urinary incontinence than men, primarily due to factors such as pregnancy, childbirth, and menopause. However, men can also develop urinary incontinence, often related to prostate problems or other medical conditions.
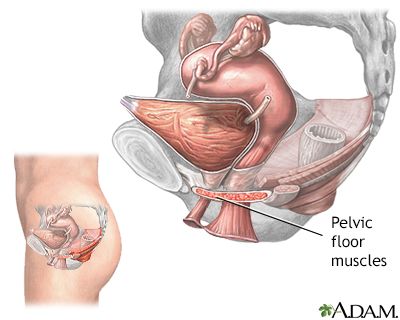
- Pregnancy and childbirth: Pregnancy and vaginal childbirth can weaken the pelvic floor muscles and damage the nerves that control bladder function, increasing the risk of urinary incontinence.
- Menopause: Hormonal changes during menopause can lead to a decrease in estrogen levels, which can contribute to the weakening of the pelvic floor muscles and urinary incontinence.
- Certain medical conditions: Conditions such as obesity, diabetes, neurological disorders, urinary tract infections, and chronic coughing can increase the risk of urinary incontinence.
- Certain medications: Some medications, such as diuretics, sedatives, and muscle relaxants, can affect bladder function and contribute to urinary incontinence.
What causes Urinary Incontinence?
Urinary incontinence can be caused by various factors, depending on the type of incontinence. Common causes include:
- Weak pelvic floor muscles: The pelvic floor muscles support the bladder and urethra. Weakening of these muscles, often due to factors like pregnancy, childbirth, aging, or obesity, can lead to stress incontinence or urge incontinence.
- Overactive bladder muscles: In some cases, the muscles of the bladder may become overactive, causing an urgent need to urinate and leading to urge incontinence.
- Nerve damage: Nerve damage or dysfunction can disrupt the communication between the bladder and the brain, resulting in various types of urinary incontinence.
- Obstruction: Conditions that obstruct the normal flow of urine, such as urinary stones, tumors, or an enlarged prostate gland in men, can cause overflow incontinence.
- Hormonal changes: Changes in hormone levels, particularly estrogen in women during menopause, can affect the strength and integrity of the urinary system, contributing to urinary incontinence.
How does Urinary Incontinence start?
Urinary incontinence can develop gradually over time or suddenly, depending on the underlying cause. It may start with occasional leakage during activities such as laughing, sneezing, or exercising (stress incontinence). Alternatively, it may begin with a sudden and intense urge to urinate, leading to difficulty reaching the bathroom in time (urge incontinence). Other types of urinary incontinence, such as overflow incontinence, may involve a constant dribbling of urine due to an obstruction or weakened bladder muscles.
What are the symptoms of Urinary Incontinence?
The symptoms of urinary incontinence can vary depending on the type and severity of the condition. Common symptoms include:
- Leakage of urine during activities such as coughing, sneezing, laughing, or exercising (stress incontinence)
- Sudden and strong urges to urinate, often accompanied by an inability to reach the bathroom in time (urge incontinence)
- Frequent urination, including waking up multiple times at night to urinate (nocturia)
- A constant dribbling of urine (overflow incontinence)
- A feeling of incomplete emptying of the bladder after urination
- Urinary urgency or a frequent need to urinate throughout the day
- Emotional distress, embarrassment, or anxiety related to the loss of bladder control
How is Urinary Incontinence diagnosed?
To diagnose urinary incontinence, a healthcare professional will typically perform a thorough evaluation, including a medical history review, physical examination, and possibly some diagnostic tests. These may include:
- Bladder diary: Keeping a record of fluid intake, urine output, and episodes of incontinence can help identify patterns and triggers.
- Urinalysis: A urine sample may be analyzed to check for signs of infection, blood, or other abnormalities.
- Post-void residual measurement: This test measures the amount of urine left in the bladder after urination to determine if the bladder is emptying completely.
- Urodynamic testing: This specialized testing assesses bladder function and measures pressure changes during filling and emptying of the bladder.
- Imaging tests: In some cases, imaging tests such as ultrasound or cystoscopy may be used to evaluate the bladder and urinary tract for any structural abnormalities or signs of obstruction.
How can Urinary Incontinence be treated?
The treatment of urinary incontinence depends on the underlying cause and the type of incontinence. Treatment options may include:
- Lifestyle modifications: Making changes to lifestyle habits can help manage and reduce urinary incontinence. This may involve techniques such as bladder training, scheduled toileting, fluid management, weight loss (if applicable), and pelvic floor exercises (Kegel exercises) to strengthen the muscles that control urine flow.
- Medications: Depending on the type of incontinence, certain medications may be prescribed to relax the bladder, reduce urinary urgency, or strengthen the pelvic floor muscles.
- Behavioral techniques: Techniques such as biofeedback, which involves using sensors to provide feedback on muscle activity, or electrical stimulation, which stimulates the pelvic floor muscles, can be used to improve bladder control.
- Devices and aids: In some cases, healthcare professionals may recommend the use of devices such as pessaries or urethral inserts to support the bladder and prevent leakage.
- Surgery: In certain situations, surgery may be considered to address structural abnormalities, such as repairing weakened pelvic floor muscles or correcting bladder obstructions.
What complications may occur with Urinary Incontinence?
Urinary incontinence can have various physical, emotional, and social complications, including:
- Skin problems: Constant moisture from urine can lead to skin irritation, infections, and pressure sores.
- Urinary tract infections: Incontinence increases the risk of urinary tract infections due to the presence of bacteria in the urinary tract.
- Impaired quality of life: Urinary incontinence can significantly impact a person's quality of life, leading to embarrassment, social withdrawal, and a loss of confidence and self-esteem.
- Emotional and psychological effects: Living with urinary incontinence can cause anxiety, depression, and emotional distress due to the fear of embarrassment or the inability to engage in social activities.
- Sleep disturbances: Frequent nighttime urination (nocturia) can disrupt sleep patterns and contribute to fatigue and daytime drowsiness.
- Limitation of daily activities: Severe urinary incontinence can limit a person's ability to participate in daily activities, work, or travel.
How can I prevent Urinary Incontinence?
While it may not always be possible to prevent urinary incontinence, there are certain steps that can help reduce the risk or manage the condition:
- Maintain a healthy weight: Excess weight can put additional pressure on the bladder and pelvic floor muscles, contributing to urinary incontinence.
- Practice pelvic floor exercises: Regularly performing pelvic floor exercises, also known as Kegel exercises, can help strengthen the muscles that control bladder function.
- Avoid smoking: Smoking can contribute to coughing, which can strain the pelvic floor muscles and exacerbate urinary incontinence.
- Stay hydrated: Drinking an adequate amount of water can help maintain bladder health and prevent urinary tract infections.
- Practice good toileting habits: Empty the bladder regularly, avoid delaying urination, and ensure complete emptying of the bladder.
- Manage chronic conditions: Control chronic conditions such as diabetes or respiratory conditions that can contribute to urinary incontinence.
- Minimize bladder irritants: Avoid or limit the consumption of bladder irritants such as caffeine, alcohol, and acidic or spicy foods.
Long-term management of Urinary Incontinence
For individuals with chronic or persistent urinary incontinence, long-term management strategies may be necessary. These can include a combination of the following:
- Continued adherence to lifestyle modifications, such as maintaining a healthy weight, practicing pelvic floor exercises, and managing fluid intake.
- Regular follow-up with a healthcare professional to monitor symptoms, assess treatment effectiveness, and make necessary adjustments.
- Ongoing use of medications or medical devices as prescribed.
- Supportive care and counseling to address emotional and psychological aspects of living with urinary incontinence.
- Accessing support groups or educational resources to learn from others with similar experiences and gain practical tips and advice.
What is recent research saying about Urinary Incontinence?
Recent research on urinary incontinence focuses on improving diagnostic methods, developing new treatment options, and understanding the underlying mechanisms of the condition. Studies explore innovative therapies, such as neuromodulation techniques and regenerative medicine approaches, as well as advances in surgical techniques. Research also aims to improve the understanding of risk factors, the impact of lifestyle interventions, and the effectiveness of different treatment modalities.
Where can I go for more information on Urinary Incontinence?
For more information on urinary incontinence, reliable sources such as the National Association for Continence, the American Urological Association, and the Mayo Clinic, can provide valuable information and resources. These sources offer comprehensive information on urinary incontinence, including educational materials, support networks, treatment options, and ongoing research updates. Consulting with a healthcare professional, such as a urologist or primary care physician, can also provide personalized information and guidance specific to an individual's situation.

