Ulcerative Colitis
What is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. It causes inflammation and ulcers in the lining of the colon, resulting in various gastrointestinal symptoms. Ulcerative colitis is characterized by periods of flare-ups, where symptoms worsen, followed by periods of remission, during which symptoms subside. It is a lifelong condition with no known cure, but with proper management and treatment, individuals with ulcerative colitis can lead fulfilling lives.
Who's at risk for Ulcerative Colitis?
Ulcerative colitis can develop at any age, but it most commonly begins in people between the ages of 15 and 30. While the exact cause is unknown, several factors may contribute to the development of ulcerative colitis, including:
- Genetic predisposition: People with a family history of ulcerative colitis have a higher risk of developing the condition.
- Immune system dysfunction: Ulcerative colitis is believed to result from an abnormal immune response, where the immune system mistakenly attacks the healthy cells in the colon.
- Environmental factors: Environmental triggers, such as certain infections or exposure to certain substances, may play a role in the development of ulcerative colitis.
- Ethnicity: Certain ethnic groups, such as Ashkenazi Jews, have a higher risk of developing ulcerative colitis.
What causes Ulcerative Colitis?
The exact cause of ulcerative colitis is unknown, but it is thought to result from a combination of genetic, environmental, and immunological factors. An abnormal immune response in individuals with a genetic predisposition appears to trigger inflammation in the colon. The immune system mistakenly identifies harmless substances, such as food or beneficial gut bacteria, as threats and launches an inflammatory response. This chronic inflammation leads to the characteristic symptoms of ulcerative colitis.
How does Ulcerative Colitis start?
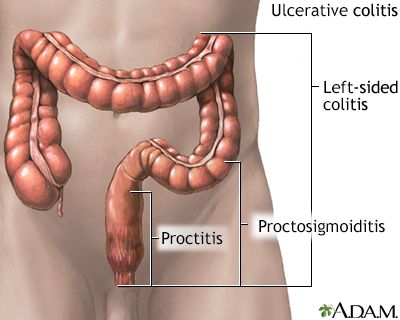
Ulcerative colitis typically starts with inflammation in the rectum and may gradually extend to other parts of the colon. The disease progresses in a continuous pattern, affecting the innermost lining (mucosa) of the colon. Inflammation causes the colon to become red, swollen, and ulcerated, leading to symptoms such as abdominal pain, diarrhea, and rectal bleeding. The disease may vary in severity, with some individuals experiencing mild symptoms and others facing more extensive inflammation and complications.
What are the symptoms of Ulcerative Colitis?
The symptoms of ulcerative colitis can vary in severity and may come and go. Common symptoms include:
- Diarrhea, often with blood or pus
- Abdominal pain and cramping
- Rectal bleeding
- Urgency to have bowel movements
- Tenesmus (feeling of incomplete bowel movements)
- Fatigue
- Weight loss
- Loss of appetite
- Anemia (due to chronic bleeding)
- Fever (during flare-ups)
In severe cases or during flare-ups, individuals may experience additional symptoms such as dehydration, severe abdominal pain, joint pain, eye inflammation, or skin rashes.
How is Ulcerative Colitis diagnosed?
Diagnosing ulcerative colitis involves a combination of medical history, physical examination, and diagnostic tests. A healthcare professional will inquire about symptoms, perform a physical examination, and review medical history. Diagnostic tests may include:
- Blood tests: Blood tests can help assess inflammation levels, check for anemia, and evaluate overall health.
- Stool sample: Analyzing a stool sample can help rule out other causes of gastrointestinal symptoms, such as infections.
- Colonoscopy: A colonoscopy allows the visualization of the colon's inner lining. During the procedure, a flexible tube with a camera is inserted into the rectum to examine the colon and obtain biopsies for analysis.
- Imaging tests: In some cases, imaging tests such as CT scans or X-rays may be performed to evaluate the extent of inflammation or complications.
How can Ulcerative Colitis be treated?
The treatment of ulcerative colitis aims to reduce inflammation, alleviate symptoms, and achieve and maintain remission. Treatment options may include:
- Medications: Various medications can be prescribed to manage inflammation, control symptoms, and suppress the immune response. These may include aminosalicylates, corticosteroids, immunomodulators, biologics, and other targeted therapies. The choice of medication depends on the severity of the condition and individual response.
- Lifestyle modifications: Making certain lifestyle changes can help manage ulcerative colitis. This may include dietary modifications, stress reduction techniques, regular exercise, and adequate hydration.
- Surgery: In cases of severe ulcerative colitis or complications that do not respond to other treatments, surgery may be necessary. Surgery may involve removing the colon and rectum (proctocolectomy) and creating an ileal pouch or a permanent ileostomy.
What complications may occur with Ulcerative Colitis?
Ulcerative colitis can lead to several complications, including:
- Severe bleeding: Chronic inflammation can cause ulcers to bleed, leading to anemia and potentially requiring blood transfusions.
- Perforation: Inflammation can weaken the colon wall, leading to perforation or the formation of abnormal connections between different parts of the intestine (fistulas).
- Toxic megacolon: In rare cases, inflammation can cause the colon to dilate and become paralyzed, a condition known as toxic megacolon. This is a medical emergency requiring immediate treatment.
- Increased risk of colon cancer: Individuals with long-standing ulcerative colitis have a higher risk of developing colon cancer. Regular monitoring and surveillance colonoscopies are essential to detect precancerous changes or cancer at an early stage.
- Malnutrition: Chronic inflammation and poor nutrient absorption can lead to malnutrition, weight loss, and nutritional deficiencies.
How can I prevent Ulcerative Colitis?
As the exact cause of ulcerative colitis is unknown, it is challenging to prevent its development. However, some strategies may help reduce the risk of flare-ups or complications:
- Medication adherence: Taking prescribed medications as directed by healthcare professionals can help manage inflammation and prevent symptom flare-ups.
- Stress management: Stress does not cause ulcerative colitis, but it can exacerbate symptoms. Managing stress through relaxation techniques, counseling, or support groups may be beneficial.
- Regular follow-up care: Maintaining regular check-ups with healthcare professionals, including gastroenterologists, can help monitor the condition, adjust treatment if necessary, and identify potential complications at an early stage.
- Healthy lifestyle: Adopting a healthy lifestyle that includes a balanced diet, regular exercise, adequate sleep, and avoiding smoking or excessive alcohol consumption can contribute to overall well-being and potentially help manage symptoms.
Long-term management of Ulcerative Colitis
Long-term management of ulcerative colitis involves a personalized approach, working closely with healthcare professionals to monitor the condition and adjust treatment as needed. This may include regular follow-up visits, monitoring symptoms and inflammation markers, optimizing medications, managing nutritional needs, and addressing any psychosocial challenges associated with the condition. Supportive care, patient education, and adherence to treatment plans are crucial for long-term disease management.
What is recent research saying about Ulcerative Colitis?
Recent research on ulcerative colitis focuses on advancing the understanding of the disease's underlying mechanisms, improving treatment options, and exploring new therapies. Studies are investigating the role of the gut microbiome in ulcerative colitis, evaluating novel medications and biologics, and exploring targeted therapies to control inflammation more effectively. Research also explores the impact of lifestyle factors, such as diet and environmental influences, on the disease.
Where can I go for more information on Ulcerative Colitis?
For more information on ulcerative colitis, reliable sources such as the Crohn's and Colitis Foundation, the American Gastroenterological Association, or reputable gastroenterology organizations and healthcare institutions can provide valuable information and resources. These organizations offer comprehensive information on ulcerative colitis, including educational materials, support networks, treatment guidelines, and ongoing research updates. Consulting with a healthcare professional specializing in gastroenterology can also provide personalized information and guidance specific to an individual's situation.

