Temporomandibular Joint Disorder
What is Temporomandibular Joint Disorder?
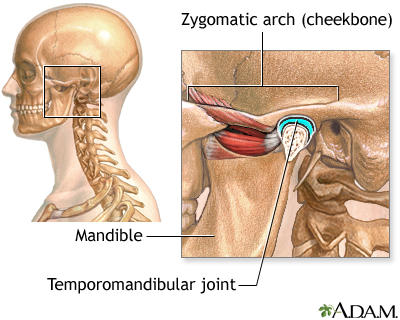
Temporomandibular joint disorder, commonly referred to as TMJ disorder or TMD, is a condition that affects the temporomandibular joint, which connects the jawbone to the skull. TMJ disorder encompasses a range of problems related to this joint, including pain, stiffness, and difficulty in jaw movement. It can affect one or both sides of the face and may cause discomfort or limitations in daily activities like eating and speaking.
Who's at risk for Temporomandibular Joint Disorder?
TMJ disorder can affect individuals of any age, but it is more commonly observed in women between the ages of 20 and 40. Certain factors may increase the risk of developing TMJ disorder, including a history of jaw injury or trauma, bruxism (teeth grinding or clenching), misalignment of the jaw or teeth, arthritis, and high levels of stress or anxiety.
What causes Temporomandibular Joint Disorder?
The exact cause of TMJ disorder is often multifactorial and can be challenging to determine. Several factors contribute to the development of this condition. Injury or trauma to the jaw joint, such as a dislocation or impact, can trigger TMJ disorder. Degenerative joint diseases like osteoarthritis or rheumatoid arthritis can also contribute to its onset. Furthermore, habits like teeth grinding or clenching, which put excessive pressure on the joint, can lead to TMJ disorder. Stress and anxiety can exacerbate symptoms, but they are not direct causes of the condition.
How does Temporomandibular Joint Disorder start?
TMJ disorder can begin gradually or suddenly, depending on the underlying causes. It may start due to an acute injury or develop over time due to chronic issues like teeth grinding or arthritis. Common initial symptoms include jaw pain, clicking or popping sounds when opening or closing the mouth, difficulty in fully opening the mouth, or a sensation of the jaw getting stuck or locked in position.
What are the symptoms of Temporomandibular Joint Disorder?
The symptoms of TMJ disorder can vary from person to person. Common symptoms include jaw pain or tenderness, particularly in the area around the temporomandibular joint. Other symptoms may include pain or discomfort while chewing, clicking, popping, or grinding sounds when moving the jaw, headaches, earaches, facial pain or fatigue, difficulty in opening or closing the mouth fully, and a feeling of the jaw being locked or stuck.
How is Temporomandibular Joint Disorder diagnosed?
Diagnosis of TMJ disorder involves a comprehensive evaluation by a healthcare professional, typically a dentist or an oral and maxillofacial specialist. The evaluation includes a detailed medical and dental history, a physical examination of the jaw joint, and an assessment of jaw movement and bite alignment. In some cases, imaging tests such as X-rays, CT scans, or MRI may be ordered to rule out other potential causes and to evaluate the condition of the joint and surrounding structures.
How can Temporomandibular Joint Disorder be treated?
Treatment options for TMJ disorder focus on relieving pain, reducing inflammation, and improving jaw function. Initially, conservative measures are often recommended, including applying moist heat or cold packs to the affected area, eating soft foods, avoiding extreme jaw movements, and practicing relaxation techniques to manage stress. Medications like nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or corticosteroids may be prescribed to alleviate pain and reduce inflammation. In some cases, oral splints or mouthguards can be used to stabilize the jaw joint and prevent teeth grinding or clenching. If conservative measures do not provide sufficient relief, more advanced interventions such as physical therapy, dental treatments, or surgery may be considered to address specific underlying causes or structural issues.
What complications may occur with Temporomandibular Joint Disorder?
In most cases, TMJ disorder does not lead to severe complications. However, if left untreated or managed poorly, it can result in chronic pain, increased jaw dysfunction, and a decreased quality of life. Some individuals may develop chronic headaches, migraines, or ear problems due to the referred pain from the jaw joint. Additionally, persistent teeth grinding or clenching can lead to dental problems, such as tooth wear, fractures, or damage to dental restorations.
How can I prevent Temporomandibular Joint Disorder?
While it may not be possible to prevent all cases of TMJ disorder, there are measures that can help reduce the risk or minimize symptoms. Maintaining good posture, avoiding excessive jaw movements, practicing stress management techniques, and implementing proper oral habits (such as not chewing on hard objects or ice) can help prevent unnecessary strain on the temporomandibular joint. Wearing a mouthguard or oral splint, if recommended by a healthcare professional, can protect the teeth and jaw joint from the effects of teeth grinding or clenching.
Long-term management of Temporomandibular Joint Disorder
Long-term management of TMJ disorder involves ongoing self-care practices and regular follow-ups with a healthcare professional. This may include the continued use of oral splints or mouthguards, practicing stress management techniques to reduce jaw tension, and maintaining a balanced diet of soft foods to prevent excessive strain during chewing. It is important to seek prompt medical attention if symptoms worsen or new issues arise. Regular dental check-ups are also necessary to monitor the condition of the jaw joint and address any dental-related concerns.
What is recent research saying about Temporomandibular Joint Disorder?
Recent research on TMJ disorder has focused on improving diagnostic methods, understanding the underlying causes, and exploring new treatment modalities. Studies have investigated the role of genetics, joint mechanics, and inflammation in the development of TMJ disorder. Additionally, advancements in imaging techniques and biomechanical analysis have contributed to a better understanding of the condition. Research is ongoing to explore the potential benefits of regenerative therapies, such as stem cell treatments, in promoting tissue repair and reducing symptoms associated with TMJ disorder.
Where can I go for more information on Temporomandibular Joint Disorder?
For more information on TMJ disorder, it is recommended to consult reputable sources such as the American Dental Association (ADA), the National Institute of Dental and Craniofacial Research (NIDCR), or the TMJ Association. These organizations provide reliable information on TMJ disorder, including symptoms, treatment options, and self-care practices. Seeking guidance from a qualified dentist or oral and maxillofacial specialist is essential for accurate diagnosis and personalized management of TMJ disorder.

